COVID-19, Metabolism & Modern Pharmacy: How a Virus Redefined Blueprint of Future Therapies
Barekat Health & Pharmaceutical Group: When COVID-19 emerged, the general and even medical consensus was that we were facing an acute respiratory illness. However, reality soon surprised us. Patients discharged from intensive care returned with symptoms seemingly unrelated to the lungs: significant weight gain or loss, type 2 diabetes, hair loss, chronic fatigue, muscle pain, mood swings, persistent insomnia, and appetite changes.
In truth, COVID-19 exerted complex effects on the body, striking the metabolic system—the heart of energy regulation, sugar, fat, hormones, and even mood. This revealed COVID-19 as a “multi-systemic impact virus,” targeting multiple vital systems simultaneously, with consequences persisting for months after infection.
This report explores a critical and practical question: Why does COVID-19 profoundly transform the body, and how has this forced the pharmaceutical industry to redefine treatments?
When the Virus Took Command of Nutrition & Energy
Our body depends on precise systems to maintain vital balance: hormones like insulin, glands such as the thyroid, receptors on cells, and enzymes in the liver and kidneys. COVID-19 invades cells bearing ACE2 receptors—from lungs to pancreas to fat cells—not only impairing respiratory function but disrupting fundamental metabolic processes, energy management, sugar and fat regulation, and even mood.
One major cause of prolonged fatigue and malaise after COVID is mitochondrial dysfunction—mitochondria being the cell’s energy factories. Patients experienced energy deficits and overeating due to misinterpreted hunger signals in the brain. Many developed insulin resistance, prediabetes, or diabetes symptoms.
Simply put: COVID-19 induced a “regulatory confusion” in the body. It couldn’t discern hunger from satiety, activity from fatigue, or health from illness.
Hidden Post-Recovery Metabolic Syndrome: Silent and Slow Diseases
Metabolic syndrome encompasses high blood pressure, increased abdominal fat, elevated blood sugar, and lipid disorders. Previously common in sedentary individuals with poor diets, post-COVID even lean, healthy people showed signs of this syndrome.
Studies found many recovered patients with elevated CRP (inflammation marker), HbA1c (long-term blood sugar indicator), and other inflammatory markers—despite feeling well. This demands a redefinition of post-COVID health: apparently healthy does not equal truly healthy.
Reprogrammed Body: How COVID Rewrote Our Biological Codes
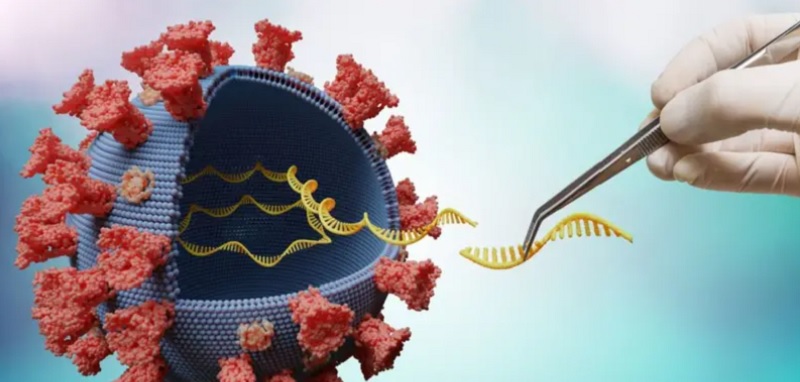
COVID-19 did more than temporarily damage systems; it reprogrammed bodies. Scientifically, stable changes in cellular mechanisms, metabolic pathways, and intracellular signaling indicate the body’s “biological code” has been rewritten—like software altered by a virus, not just broken but fundamentally changed.
Research shows COVID altered gene expression regulation in some stem cells and modified insulin responses, fat storage, and ATP (cellular energy) production. This means some patients’ bodies remain altered post-infection: more obese, less energetic, more anxious, and resistant to previous medications.
Post-COVID Bodies Demand Treatments Aligned with Cellular Reprogramming
Traditional medicine is no longer sufficient. Post-COVID bodies need therapies compatible with these cellular rewrites, such as:
-
Supplements enhancing mitochondrial function (e.g., PQQ, CoQ10);
-
Drugs targeting chronic inflammatory pathways;
-
Epigenetic drugs that directly modulate gene expression (currently under research).
Simply put: COVID did not merely cause illness; it reset the body’s systems. Treating this body requires addressing its “new code,” a challenge pharmaceutical science must be prepared for.
Inadequate Drugs, New Treatments: Need for a New Generation of Therapeutics
How did the pharmaceutical industry respond? Initially, focus was on vaccines and antivirals. Gradually, attention shifted toward managing metabolic complications. Current projects aim to develop combination drugs targeting multiple pathways: reducing inflammation, improving insulin sensitivity, and boosting mitochondrial function.
Drugs like Metformin (anti-diabetic), NAC (antioxidant), and even anti-aging compounds (Rapamycin, Resveratrol) are being investigated for long COVID treatment.
This reflects a broader shift: COVID forced a redefinition of chronic and adjunct therapies.
Clinical Reconstruction: When Science & Pharma Had to Rethink the “COVID Body”
Research centers worldwide now view COVID-19 not only as an acute infection but as a biochemical disruptor. This has led to a new branch of pharmacology—”post-viral pharmaceutics”—designing drugs not to combat the virus directly, but to restore the body after viral damage.
Part of this research leverages AI to predict drug interactions, identify optimal combinations for post-COVID bodies, and detect early metabolic disorder markers.
A Pandemic That Forced Us to Rethink Human Body
On a deeper level, COVID-19 offered an opportunity to revisit our concept of health. Previously defined as “absence of disease,” we now understand a person can appear symptom-free yet harbor metabolic dysfunction.
COVID taught us the human body is an integrated system, not just a collection of isolated organs. This insight drives the pharmaceutical industry toward more multidimensional, personalized, and intelligent treatments.
Pharmaceutical Science Is Writing a New Prescription—Not Just for COVID, but for Understanding the Complex Human Body
COVID-19 may no longer be as deadly, but it remains as a metabolic memory in millions worldwide. Pharmaceutical science today is crafting new therapies that address root causes—from cellular function to mental balance.
COVID forced us to read the body anew—with precision, science, and humility.
-
Afghanistan’s Ministry of Public Health Delegation Meets Barkat Pharmaceutical Group Executives

-
Voice of Life in World of News — Redefining Health Journalism in the Information Age

-
Senior Health Officials & Barkat GD Visit Sobhan Oncology

-
Barkat Group specialized meeting

-
Safa Appointed as Barekat General Director

-
Barekat Health & Pharmaceutical Group at the 10th Iran Pharma Exhibition

-
Ali Safa visits Sobhan Oncology & Sobhan Darou

-
Pirsalehi & Safa visit Saman Daroo 8 Knowledge-based Company

